
Volume 7 Issue 4, February 18, 2020
Integrated care is one of the big buzz words in the human services industry. Integrated care is fundamentally the combination of primary healthcare and mental healthcare in a single setting for the purpose of creating a team-based approach to general and mental care. As managed care becomes more commonplace in human services, payers are pressing for its providers to achieve the objectives of integrated care. As a result, providers are finding themselves tasked with the challenge of further decreasing cost while improving outcomes for those receiving support services. They're also wondering: What value can I provide?
There is empirical data showing that when people achieve improvements in physical health, there is inevitably greater satisfaction with their quality of life and goal completion. This is the basic principle behind the push for integrated care by managed care companies that have a focus on minimizing expenses while increasing the quality of care (which further contributes to lower healthcare costs). The fervor surrounding integrated care can make one feel a bit overwhelmed. The good news for human services providers is that this does not need to be the case if you keep in mind that we have essentially provided integrated care for many, many years.
In the mid-1990s, the Robert Wood Johnson Foundation (RWJF) set out to address the serious problems facing state programs serving individuals with developmental disabilities. They identified these problems: "… rapidly rising costs for services, insufficient resources to serve everyone who needed help and fixed sets of services that gave individuals and their families little control over what services were provided, when or how." Note: These continue to be issues today.
The RWJF initiative focused on teaching providers about self-determination for persons with developmental disabilities and those who support them. The work of this program empowered individuals receiving support and their families to have a greater say in what services were provided and how. This culminated with a person-centered plan and system to address the whole person and how best to deliver services.
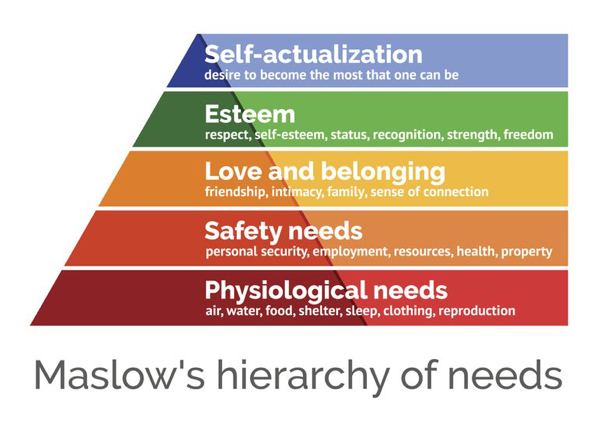
As services began to mature and a higher accountability for goal outcomes began to grow, further research was conducted to try to determine if the system was working. Through efforts such as National Core Indicators (NCI), researchers began to collect data on social determinants of health, including feeling safe, opportunities for choice, and levels of independence among those receiving support through state systems. Although there are too many points of data collected by NCI to mention here, they can be understood by examining Maslow's hierarchy of needs.
Maslow's hierarchy, a motivational theory in psychology, encourages us to answer the question: Are we starting with basic human needs and helping to build upon each level to encourage independence and social inclusion? It highlights the importance of addressing an individual's fundamental human needs before addressing more advanced emotional and social skills.
Integrated care, as we discuss it today, is a worldwide trend in healthcare focusing on more coordinated and integrated forms of care provision. People with co-occurring diagnosis may die decades earlier than the average person with contributing factors that include untreated and preventable chronic illnesses (e.g., hypertension, diabetes, obesity, cardiovascular disease) aggravated by poor health habits. As the National Institute of Mental Health notes, "Addressing the whole person and his or her physical and emotional health is essential for positive health outcomes and cost-effective care. Many people may not have access to mental health care or may prefer to visit their primary health care provider. Combining mental health services/expertise with primary care can reduce costs, increase the quality of care, and, ultimately, save lives."
Major obstacles to proper care — and thus progress within Maslow's hierarchy — include barriers to primary care and behavioral/emotional health services, together with the challenge of navigating increasingly complex and often fractured healthcare systems. If we are not addressing the basic health/emotional care needs of an individual, then we are trying to build on an unsteady foundation and are often unsuccessful in the growth of and progress toward goals.
A case can be made that a solution lies in achieving integrated care, since it's the systematic coordination of behavioral, cognitive, and general healthcare needs. Through integrating mental health, substance abuse, and primary care services, one can see how providers would be in a strong position to deliver personalized services that achieve optimal outcomes for people with multiple healthcare needs while driving costs down.
Now that we have established a baseline understanding of integrated care, let's discuss how your agency can deliver it for those managed care organizations expecting it. The path forward is simple: You must know the people you are supporting and cater to their very individualized needs. Managed care wants an experienced network of providers to deliver the necessary services while ensuring a high level of comfort for the individuals and their support systems receiving services. As you build integrated care plans, you will find yourself better equipped to identify community resources that can help support goal achievement. And as the person coordinating the individual's services, you are in the best position to identify the ways to most effectively and efficiently improve outcomes while showing a commitment to minimizing expenses.

If the idea of reducing expenses has you looking at your financial records and wondering where you can possibly cut more costs, don't worry: That's not quite what managed care is looking for.
Let's take a step back and consider everything we've been trying to do for years in the human services industry, starting with understanding social determinants of health. Begin with your care plan and think about the whole person. We tend to start with a top-down approach of Maslow's hierarchy, trying to take into consideration the ultimate goal for this person by, for example, establishing the objectives of increased community integration and independence. With that goal in mind, consider the basic level of human needs: Does this person feel safe? Do they have clothing that feels comfortable? Do they have the means to sleep adequately? Are there other fundamental quality-of-life needs being met? We often find that by completing such an exercise, we can identify barriers to the ultimate goal. Then, by addressing these barriers, we have a greater chance for success. These obstacles are often tied to areas considered "integrated," such as the need for additional physical health objectives or increase in behavioral supports.
We also know that by being proactive with physical or emotional health needs, we can bring people closer to achieving the established goals. By increasing the self-esteem, personal value, feeling of strength, and freedom of an individual — improving outcomes in the process — we will likely see a decrease in cost of care due to fewer doctors' visits, reduced depression, and/or better self-care. It goes back to the old adage: "If you feel good on the inside, you will feel better on the outside."

Any big change to our industry tends to create a lot of anxiety for those who have provided services a particular way for years. Sometimes seemingly new changes are just the return to something old. That is the case for integrated care. Managed care might be the new funder, but that does not mean we should drastically alter how we approach service delivery. Consider another adage: "If it ain't broke, don't fix it."
Direct service providers are uniquely positioned to move the needle, armed with best practice knowledge and keen insight into the culture and needs of those communities receiving support. If you have focused on creating goals that specifically targeted people receiving services, and if you have worked to improve the lives of others, then you are already keenly aware of what is required for person-centered planning. It's not you who needs managed care, but managed care is what needs you!

As Co-Founder of LifeShare, a multi-state human services and healthcare organization, Rachel has a unique background of over 20 years of successful operational and executive experience, in addition to an MBA in Healthcare Management. She began her professional life as a home care provider, an experience that created the foundation for the innovative quality and success of LifeShare, while also changing her life. At LifeShare, she managed their Operations (Adult Day/Residential; Child Therapeutic Foster Care; HCBS; Child Therapeutic Day/Diversion Services, and Educational Programming), Finance, HR and Quality Assurance (facilitating COA accreditation and policy/procedure implementation). After selling LifeShare to Centene, Rachel remained during the transition of management and helped to provide outcome measurements and COA compliance reporting. At VERTESS she is a Managing Director providing M+A advisor and consultant services, specifically in the I/DD, behavioral health and related healthcare markets, where systems are rapidly evolving, and providers are striving to adapt strategically to diverse challenges.